How to Diagnose a Concussion/mTBI
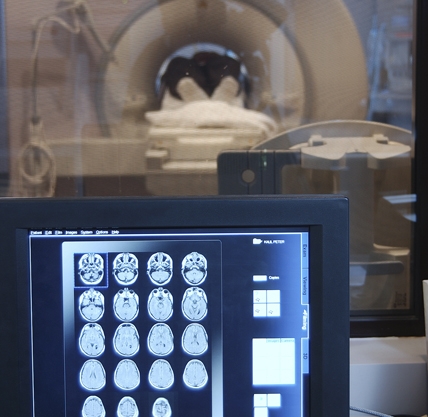
When you see a patient who has sustained a concussion/mTBI, you're going to make your diagnosis primarily based on patient history. (Remember, concussion/mTBI injuries are not typically visible with standard brain imaging techniques.) Under most circumstances, the concussion/mTBI will have occurred a long time before you actually see the patient, which can affect how much detail your patient can recall. As mentioned previously, concussion/mTBI is diagnosed by one or more of the following signs immediately after a traumatic blow or jolt to the head:
- Loss of consciousness for less than 30 minutes
- Loss of memory for events before or after the injury resolving within 24 hours
- Alteration of consciousness (confusion, disorientation, or dazed feeling) resolving within 24 hours
IMPORTANT: While a loss of consciousness is sufficient for a diagnosis of concussion/mTBI, it is not necessary.
Up to 85% of traumatic brain injuries are mild. A TBI is classified as mild if the alteration of consciousness (including amnesia) has resolved within 24 hours of the trauma. If the patient lost consciousness, the period of unconsciousness must be less than 30 minutes for the designation concussion/mTBI.
